


PHOTO CREDIT: Mayo Clinic
Biomedical Research News
-
Researchers at the Broad Institute and MIT Develop Primers to Improve Liquid Biopsy for Cancer Detection and Monitoring
January 29, 2024
Scientists from the Gerstner Center for Cancer Diagnostics at the Broad Institute and their colleagues at MIT have developed two agents that could one day be given to patients shortly before a blood draw to allow physicians to better detect tumor DNA using liquid biopsy. Liquid biopsies have the potential to transform how cancers are diagnosed, monitored, and treated by detecting DNA that tumors shed into the blood, but the body presents a significant challenge. Immune cells in the liver and DNA-degrading enzymes in blood remove circulating tumor DNA from the bloodstream within minutes, making this DNA difficult to capture and detect in a blood test. Now, researchers at MIT and the Broad Institute have developed injectable "priming agents" that enhance liquid biopsy accuracy. These agents, using nanoparticles and antibodies, significantly increase the detection of circulating tumor DNA (ctDNA) in the bloodstream. In mouse trials, these agents boosted ctDNA by over 10 times, improving the detection rate from below 10% to over 75%. This breakthrough could not only transform cancer diagnostics but also holds promise for other health areas. Director of the Gerstner Center for Cancer Diagnostics, Viktor Adalsteinsson shared “Boosting circulating tumor DNA in blood is just the tip of the iceberg… Priming is a new frontier we’re excited to further develop in cancer diagnostics and beyond.”
Read More at theBroadInstitute.orgRead More at Science.org
-
The Broad Institute Receives an Additional $20M to Support the Gerstner Center for Cancer Diagnostics
November 13, 2023
Gerstner Philanthropies has committed an additional $20 million to the Gerstner Center for Cancer Diagnostics at the Broad Institute. This commitment will support the development and optimization of liquid biopsy technology to enable more precise cancer care for millions worldwide. Directed by Dr. Viktor Adalsteinsson, this technology allows physicians to detect cancer cells and cancer recurrence, earlier than ever before. “We always knew that detecting cancer recurrence with a blood test would be an incredible feat, and the scientists in the Gerstner Center have risen to the challenge," said Todd Golub, director of the Broad Institute. This development for early detection is key to measuring patients’ response and assessing treatment options. “I first partnered with the Broad to launch the Gerstner Center in order to impact clinical care for cancer patients, and I’ve been pleased to see that Viktor and his team have created an engine of innovation that could transform not only cancer treatment but possibly other fields as well,” said Gerstner.
Read More at Broadinstitute.org
-
GSK Awards 2023 Chairman’s Prize
 August 16, 2023
August 16, 2023Chi Nguyen, a PhD student attending the Gerstner Sloan Kettering Graduate School of Biomedical Sciences (GSK), has been awarded the 2023 Chairman’s Prize. The $2,000 prize recognizes Nguyen's research on interactions between environmental factors, gut microbiota, and the immune system in acute graft-versus-host disease following allogeneic hematopoietic cell transplantation (allo-HCT). “Microbiota” refers to the fungi, bacteria and viruses that live in the intestines and play a pivotal role in regulating the immune system. Little is known about how different medications can impact this microbiota. Nguyen’s research aims to give physicians a better understanding of how they can protect the gut health of patients with cancer while they are undergoing treatment. Nguyen conducted her research under the mentorship of Marcel van den Brink, MD, PhD, Head of the Division of Hematologic Malignancies, who also has a lab in the Immunology Program at the Sloan Kettering Institute (SKI). Of her research, Dr. van den Brink shared: “Chi was very brave to engage in this project, which was purely computational biology. Her background in this field was limited when she joined my lab. Therefore, I am even more proud of her accomplishments.” Nguyen was born and raised in Hanoi, Vietnam, and moved to the United States to attend Colgate University in Hamilton, New York. In 2018, after graduation, she moved to New York City to pursue graduate school with an eye on cancer research. “My parents have always inspired a sense of curiosity in me,” says Nguyen. “Curiosity about the natural world, biology, and how things work.”
Read More at MSKCC.org
-
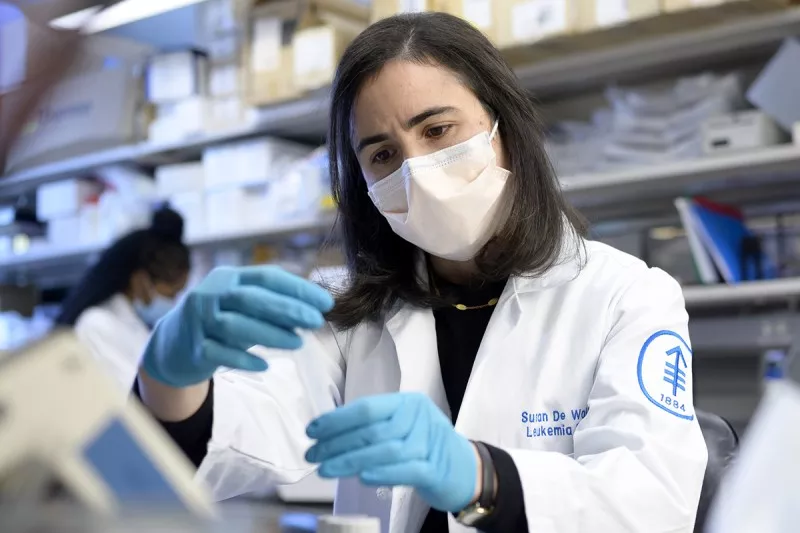
Mayo Clinic Names 2023 Recipients of Gerstner Family Career Development Awards
August 2, 2023
The Mayo Clinic has announced the 2023 recipients of the Gerstner Family Career Development Awards. These awards are presented annually to researchers conducting innovative investigations to predict, prevent, treat, and cure diseases using individualized medicine approaches. This year, physician scientist Patrizia Mondello, M.D.,Ph.D., M.Sc., and medical oncologist Ryan Carr, M.D., Ph.D., have been selected to further develop their research in treating follicular lymphoma and pancreatic cancer resistance, respectively. For these studies, both of which aim to improve the outcomes for patients facing resistant forms of cancer, securing funding in these earliest stages is crucial.
Read More At: MayoClinic.org
-
MSK 2022 Annual Report: The Special Calling of Physician-Scientists at MSK
 June 27, 2023
June 27, 2023As highlighted in their newly released annual report, Gerstner Philanthropies is working with Memorial Sloan Kettering (MSK) to support early career physician-scientists launch careers in the face of the unique challenges that come with juggling the rigors of clinical care and laboratory research. “The development of the Gerstner Physician Scholars Program is critically important to address the shortfall of cancer subspecialists who are highly trained as experts in both clinical care and scientific research, and who can translate their findings from the bench to the bedside, and back,” says Monika Shah, MD, Deputy Physician-in-Chief of Education and Faculty Affairs at MSK.
Read more at mskcc.org

